Understanding fibrosis, at the heart of many diseases
Categories : Recherche Talents
paru le 02-01-2021 (16:10) - Updated on 10-29-2024 (15:57)
Characterised by hyperactivity of the body’s defence system, the study of chronic inflammatory diseases is the specialty of the Infinite¹ research unit. The latter has just been awarded a highly prestigious label for three years, that of the Foundation for Medical Research. ‘This is truly a label of excellence: the call for tenders is extremely competitive, and the selection committee is of the highest calibre’,says laboratory director Laurent Dubuquoy. ‘Moreover, it is rare for teams working on inflammatory diseases to receive this kind of accreditation’, adds David Launay, the laboratory’s deputy director and a specialist in internal medicine, evidently delighted.
The Medical Research Foundation awards this label to topics it considers to be important and strategic for medical research in the years ahead. ‘This prompted us to submit a truly innovative project’, says Laurent Dubuquoy. The project is original in two respects. Firstly, because it aims to analyse several inflammatory diseases at the same time, even though they seem to have little in common, affecting a particular organ or, conversely, the whole organism. This project focuses on scleroderma, chronic inflammatory bowel disease and alcoholic hepatitis.
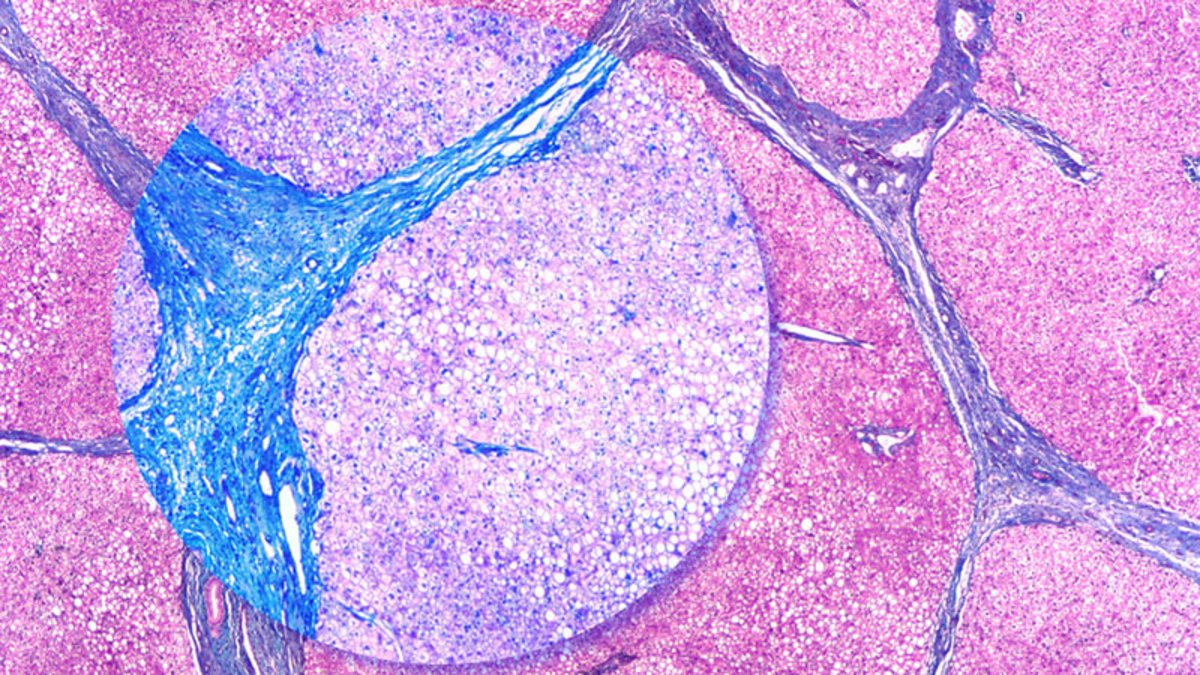
For these seemingly very different diseases have one thing in common, which the project has decided to focus on: they often progress to a major complication, fibrosis, with sometimes dramatic consequences. It is responsible for a significant number of deaths worldwide, because it can occur during the course of many common pathologies (affecting the heart, lungs, liver, kidneys, etc.).
Fibrosis is a healing process that goes ‘off the rails’, so to speak. Somewhere in the body, a disease tends to destroy biological tissue. ‘But the tissue generated by the body for repair is not functional’,explains Laurent Dubuquoy. ‘As a result, if fibrosis affects a large part of an organ, it may no longer function.’
Scientific and medical teams know very little about the mechanisms that regulate fibrosis. In the past, most of the time, they only approached the latter from the perspective of the particular pathology in which it occurs. ‘The aim of our project is to identify the mechanisms that are common to these pathologies, and those that distinguish them from one another’,explains Laurent Dubuquoy. ‘Not only to advance knowledge, but also to identify therapeutic targets from which new medications can emerge.’
Treatments for inflammatory diseases have reached a dead end, because they tend to focus only on the initiator of fibrosis, chronic inflammation. ‘Until now, the tendency has been to develop treatments only to combat chronic inflammation, with the prevailing opinion being that once the fibrosis stage had been reached, it was too late’,explains Laurent Dubuquoy. ‘But these treatments are rarely curative, probably because fibrosis rapidly acquires a kind of ‘autonomy’ from the inflammation that causes it.’ Hence the importance of looking at fibrosis itself, to unravel its complex relationships with tissue regeneration and inflammation in order to identify new treatments.